Spinal Cord Injuries (SCI) involve damage to the nerves of the spinal canal. These nerves allow our brains to communicate with the rest of our bodies and include control of motor function and sensory perception, including those vital functions like breathing and blood pressure. An injury to the spinal cord blocks or disrupts these messages.
to communicate with the rest of our bodies and include control of motor function and sensory perception, including those vital functions like breathing and blood pressure. An injury to the spinal cord blocks or disrupts these messages.
The severity of SCI depends on the site of the injury on the spinal cord and the severity of the injury. Motor and sensory function is affected below the level of injury. A SCI at the level of the neck will result in tetraplegia (quadriplegia) which affects movement and sensation in all four limbs, the pelvic organs and muscles of the trunk. An SCI in the back will affect movement and sensation in the lower limbs, pelvic organs and possibly some lower trunk muscles. Injuries can be described as complete or incomplete SCI. Simply put, a complete SCI means no nerve messages are conveyed past the site of the injury, whereas incomplete SCI can have some messages passing through the site of injury.
There is a higher prevalence of SCI in young adults and males. Causes include trauma (such as road traffic accidents, sports related injuries, gunshot wounds), infection or disease. Additional damage can occur after the actual injury due to bleeding, inflammation and pressure on the spinal cord. Almost all persons with SCI will have neurological impairments, motor loss and sensory loss to a varying extent.
SCI can result in loss of muscle strength, sensation, body functions below the level of the injury (for example: respiratory function, bladder and bowel control, reduced sexual function). Muscles can atrophy from non-use, they can spasm and become tight (high tone/spasticity), be paralysed and relaxed (low tone). Individuals can experience sudden changes in their blood pressure, and potentially have autonomic hyperreflexia (sudden increase in blood pressure) which can be life-threatening. There are associated risks of further fractures after SCI (Gifre et al., 2014) and pressure related injuries due to immobility and reduced/lack of sensation over load-bearing body areas. Pain, fatigue, low mood and psychosocial changes are also common following SCI.
SCI clients able to walk with mobility aids or with support may experience disabling fatigue, increased pain, increased need for assistance to mobilise (either by a person or equipment) and depression (DiPiro et al., 2014). For some a wheelchair may be required intermittently to enable participation and function when pain and fatigue restrict ambulation. For others, a wheelchair is a permanent necessity for mobility.
Pain can develop from using muscles in different ways and can also be due to nerve pain (especially for incomplete SCI). Pain can also be particular to the shoulders and wrists of those who self-propel their wheelchairs (Siddall & Loeser, 2001) – the arms take over the role of mobility when self-propelling manual wheelchairs, but this can result in significant fatigue, shoulder and wrist pain (Barbetta et al., 2016; Siddall & Loeser, 2001). Options for mobility include self-propulsion using the arms and powered wheelchair control options.
Many individuals with SCI may continue to drive their own vehicles with some adaptation, and this has an impact on the wheelchair selection. Accessing the wider the community for all wheelchair users is a key consideration for maintain and improving on quality of life post-injury.
When considering seating provision for individuals, the key elements need to include:
- Providing appropriate pressure relief.
- Providing support and positioning to minimise fatigue.
- Facilitate engagement in functional activities and promote independence, including propelling the wheelchair, accessing transport and the wider community.
- Supporting the body to maintain a healthy alignment against gravity at the hips, trunk and head.
- Optimise posture for cardiac, respiratory and gastrointestinal function.
- Allow for independent and assisted transfers, as appropriate.
- Be aesthetically pleasing and allow for self-expression.
- Adequate support to the pelvis and trunk to provide stability.
- Adequate support to the arms and head for higher level injuries.
- Protection of body parts with limited sensory feedback.
- Be easy to use by client and family/carers.
- Provide comfort.
Spex seating is a versatile, adjustable modular system that can be fixed onto almost any wheelchair chassis. It can be easily transported.
chassis. It can be easily transported.
Paediatric, kids and adult seating technology ranges can grow and adapt to the users’ needs as they experience changing needs. Users only need order what they need and can add/remove components as their condition changes.
Spex provides support to active users and to users who require greater levels of support and shaping for comfort. Spex is customisable to reflect personal colour choice, quick to adjust and includes the ability to support complex postures.
Spex shapes better lives and supports functional engagement!
Spex Seating Technology Products
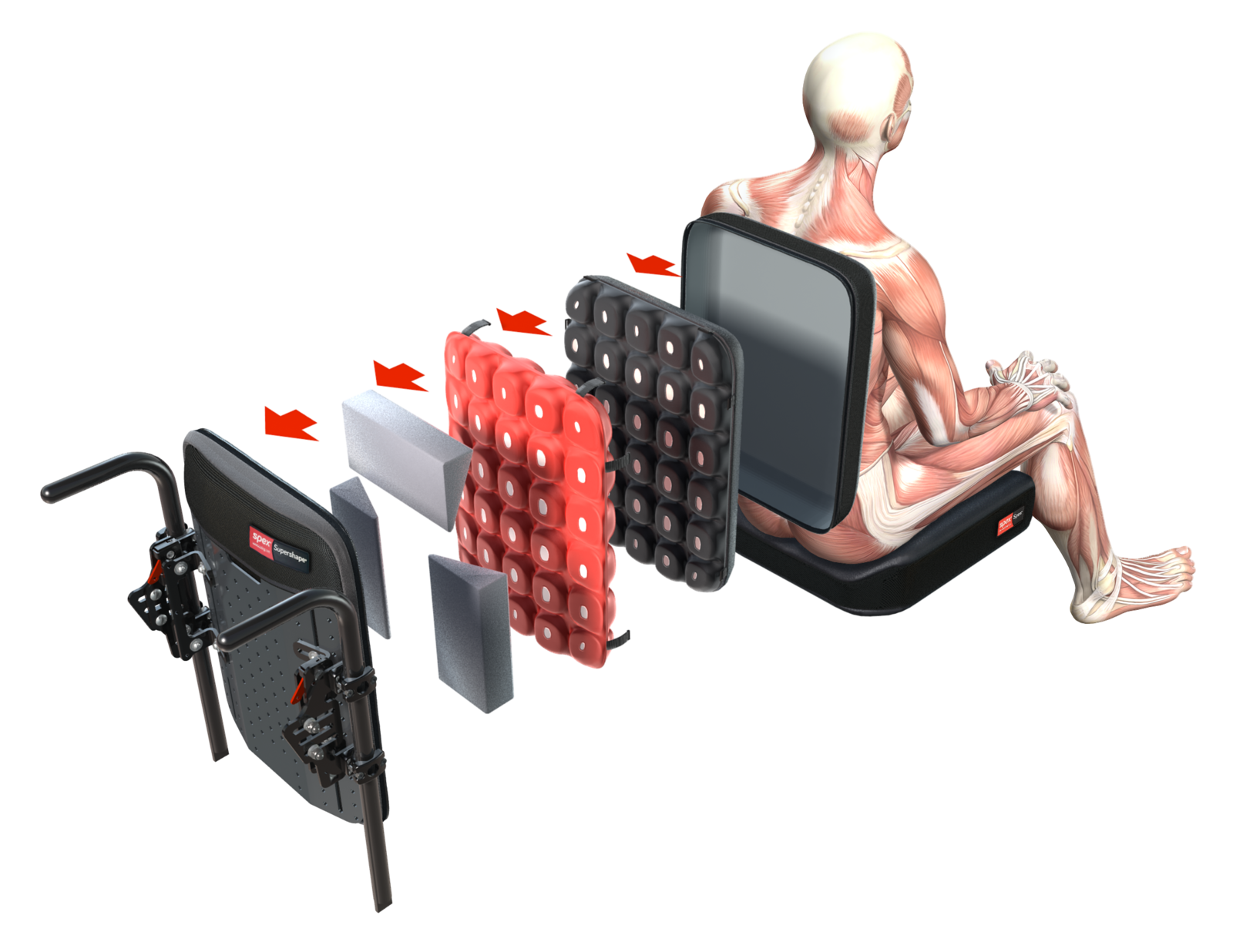
Spex for kids and adults is a modular seating technology system that includes cushions, hip supports, trunk supports, knee/thigh supports, head and arm supports, a variety of accessories, and back supports that can allow for easy adjustment and contouring and shaping within the cushions and back supports. The seating systems fit onto almost any wheelchair chassis (manual and powered wheelchair chassis options) and can be removed for easy transportation.
Items can be used in isolation or as a full seating system on their chosen wheelchair chassis base. The mix-and-match componentry allows for products to work together based on need, level and direction of support required and the user’s functional requirements. Users only need order what they need and can add/remove components if their condition changes.
The seating options allow for active wheelchair use and self-propulsion, as well as more immersive and shaped options to accommodate the need for additional stability and postural support. Spex is customisable to reflect personal colour choice, quick to adjust and modular to provide the right support when needed.
Spex Back Support Range
Spex Vigour
The Spex vigour range includes the lo, mid and high back support. These are tailored for the more active users to allow free upper limb movement. Being angle-adjustable and light-weight, with additional positioning kits for shaping as required, these supports offer a versatile positioning and support to meet individual need.
Quick release mounts allow for easy transportation.
Ideally suited to active users requiring sacral and lumbar support with unrestricted upper body movement.
Spex Manta
The Manta provides lateral support to users with mild trunk asymmetries without compromising upper limb movement by adding additional hardware for lateral support. The lateral ‘wings’ can be minimally adjusted.
It is lightweight and provides greater support that the Vigour range. Additional shaping can be provided with positioning kits if required and if greater support is needed for the head, a head support can be fitted with ease.
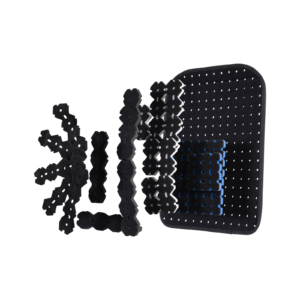
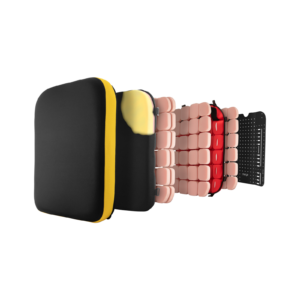
Spex Tessellated Positioning Kit
Some active users may require additional shaping and contouring of the supports at the trunk without compromising the weight of the wheelchair.
The tessellated positioning kit can sit behind the Spex upholstery to allow for shaping to the user to optimise support, without compromising on comfort and weight. It allows customisations and adjustment.
Spex Height-Adjustable Shell
The height-adjustable shell option incorporates inbuilt growth adjustment in the back support due to the upper sliding interface.
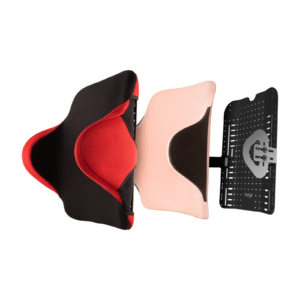
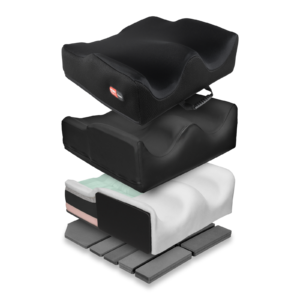
Spex Shape and Spex Supershape Back Supports
The more supportive Spex and Spex SuperShape are versatile back supports that respond quickly (with easy adjustment) to more complex postural changes including posterior pelvic tilt or obliquity, spinal scoliosis, pre-/post-surgical needs and asymmetry.
These back supports allow for greater immersion, pressure redistribution and support by adjusting the shaping within the upholstery to ensure optimal conformity and support to the user without compromising on pressure distribution and comfort.
Spex Head Support
The Spex head support range provides support in several different positions to provide optimal head alignment to encourage interaction, manage fatigue and pain and promote continued engagement in activities.
The range includes the basic compact head support for users with good head control, the square head support, the contoured and the adjustable lateral head support for greater support needs.

Spex Trunk, Hip and Medial Knee/Thigh Supports and Accessories
The Spex lateral trunk supports, hip and medial thigh/knee supports included patented axial technology that can respond to the user’s unique postural presentation and need.
There are various sizes to suit individual need. There is a range of pelvic support belts and thoracic support harnesses to optimise stability, posture and position within the seating system.
With various mounting solutions, the configurations can be adjusted to promote safety with chosen transfer methods.
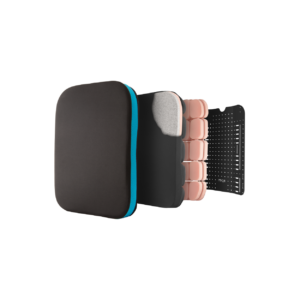
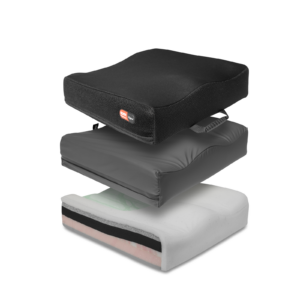
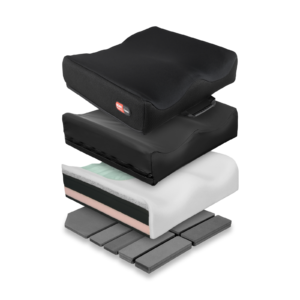
The Spex Vigour cushions provide a contoured cushion to promote comfort and posture.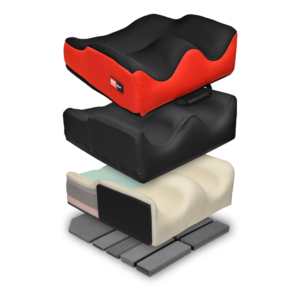
The Spex contour cushions (Standard contour, High contour and SuperHigh contour) have additional features allowing for shaping to the more complex postural presentation to promote stability at the pelvis, hips and thighs and promote comfort and pressure relief whilst influencing trunk alignment.
Increased shaping allows for improved stability, reduced effort to sit to reduce fatigue, management of asymmetry and comfort for the user.
Cushions include both an incontinence cover and a fabric breathable layer to promote breathability and support pressure management needs. All cushions have an inherent Velcro fabric over the base to securely fix onto seat pans.
Contact us to:
- Arrange clinical education on our products in your venue of choice, or
- Obtain information about your local dealer for sales enquiries if outside of New Zealand & Australia.
Barbetta, D. C., Lopes, A. C. G., Chagas, F. N. M. R., Soares, P. T., Casaro, F. M., Poletto, M. F., … Ogashawara, T. O. (2016). Predictors of musculoskeletal pain in the upper extremities of individuals with spinal cord injury. Spinal Cord, 54(2), 145–149. https://doi.org/10.1038/sc.2015.126
DiPiro, N. D., Saunders, L. L., Brotherton, S., Kraft, S., & Krause, J. S. (2014). Pain and fatigue as mediators of the relationship between mobility aid usage and depressive symptomatology in ambulatory individuals with SCI. Spinal Cord, 52(4), 316–321. https://doi.org/10.1038/sc.2013.164
Gifre, L., Vidal, J., Carrasco, J., Portell, E., Puig, J., Monegal, A., … Peris, P. (2014). Incidence of skeletal fractures after traumatic spinal cord injury: a 10-year follow-up study. Clinical Rehabilitation, 28(4), 361–369. https://doi.org/10.1177/0269215513501905
Siddall, P., & Loeser, J. (2001). Pain following spinal cord injury. Spinal Cord, 39, 63–73.
Tsai, I.-H., Graves, D. E., & Lai, C.-H. (2014). The association of assistive mobility devices and social participation in people with spinal cord injuries. Spinal Cord, 52(3), 209–215. https://doi.org/10.1038/sc.2013.178