Click on the link below to get your copy of Paul’s notes on the Clinical Benefits of Standing, presented at the ATSA Independent Living Expo at Melbourne in May.
Early Intervention
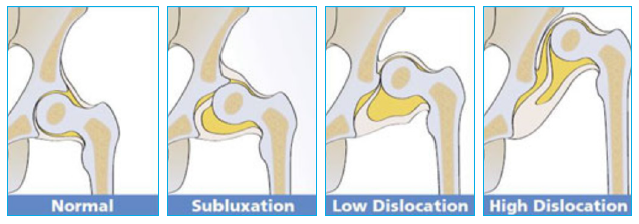
- Maintaining a healthy hip joint
- The importance of standing in abduction
- Children who stand at the normal development age of 12-16 months are more likely to form a healthy femoral head and acetabulum groove (1)
- During birth to 3-4 years of age weight bearing and movement are critical to bone development
- Long bones continue to grow into late teens with puberty spurts and growth plates don’t usually fuse until 17 – 20 years of age
- Neurological conditions such as cerebral palsy can impact on these development milestones in the following ways:
- Delayed bone development
- Delayed weight bearing
- Decreased movement
- Presence of Abnormal tone – high or low
- Children with a GMFCS of IV or V are most at risk of hip subluxation/dislocation with a prevalence of between 68 – 90% of this population (2)
- Children at risk of hip subluxation/dislocation should begin a standing programme between 8 -12 months of age (3)
- There is no “cut off” age for implementing a standing programme and it is just as important for a teenager/adult to stand daily as a child (3)
- Most published clinical research is based on standing with 60° overall abduction (4)
- Questions remain around why 60° was the chosen range (4)
- Yet to be published study by the Pearlman Centre in Cincinnati suggests that 30° of overall hip abduction has the same clinical impact as 60°
- Standing in abduction increases the opportunity for the head of the femur to locate into the acetabulum groove
- The amount of abduction should always be governed by the tolerance levels of the child
- Constant monitoring of hip health is integral to managing hip health and adjusting the standing programme to meet the best outcomes
- As a guide the following are ideal ranges of hip position and dosage
| Child’s Age | Hip Position | Dosage |
|---|---|---|
| 0 – 2 years | Minimum 15° each leg | Use daily as per infant’s tolerance (5) |
| 2 – 6 years | 15 – 30° each leg (5,8) | 60 – 90 minutes per day (6,7) |
| 6 to skeletal maturity | 15 – 30° each leg (8) | 60 – 90 minutes per day |
- Upright – Ideal for children who require lower limb stability and minimal trunk support
- Prone – Use with children who have poor but developing head control – ideal to use after “Tummy time” prone lying has shown some active neck extension
- Supine – For children who have poor head control with no indication of progress through therapy or where knee flexion is too extensive to comfortably accommodate in prone.
- Consider factors outside of the clinical objectives such as home environment, parents abilities and cultural barriers
- If it is unclear how a child will progress consider opting for a 3 in 1 standing frame which offers the ability to swap between Prone, Supine and Upright positioning
- Consider equipment that allows the child’s standing angle to be easily adjusted whilst the product is in use
- The length of a standing session can be extended by altering the angle of the frame to a more restful position as the child fatigues
- This feature also allows for the child to be challenged against different levels of gravity to work on conditioning – especially prevalent in building head control
- If the child is objecting to standing consider using a standing frame which offers a large range of prone angle adjustment so that a “Tummy time” position can be replicated to build tolerance of the product (Prone positioning only).
- Look to steadily increase the angle to a more weight bearing position
- Consider equipment that allows for active therapy during standing
- Easy tray height and angle adjustment
- Allows for different amounts of upper extremity support, this can have a significant impact on head control
- Allows opportunity to practice hands to midline
- Promotes reach and grasp fine motor control
- Easy height adjustable lateral supports
- Allows support to be temporarily removed to encourage the child to experience their body in space* assessment
- Alternatively, can offer more support for targeted activity that requires extra stability
- We know that one of clinical benefits of standing is postural drainage, particularly bowel and bladder emptying under gravity. Ensure the product you choose has easily to wipe clean covers!
- Standing needs to part of a 24 hour postural management programme
- Every child is different and their abilities can vary on a daily basis – be prepared to adapt
(1) Labandz 2011
(2) Soo B, Howard J, Boyd R, et al. Hip displacement in cerebral palsy. J Bone Joint Surg Am. 2006
(3) Melissa Tally, Erin Pope, 2013 – formulating proper dosing for standing
(4) Martinsso & Himmelmann, 2011; Macias-Merlo, Bagu-Calafat, Girabent-Farrés, & Stuberg, 2015; Macias-Merlo, Bagu-Calafat, Girabent-Farrés, & Stuberg, 2015
(5) Paleg, Smith and Glickman, 2013 – Systematic review and evidence based clinical recommendations for dosing of paediatric supported standing programmes
(6) Martison and Himmelman, 2011 – Effect of weight bearing in abduction and extension on hip stability in children with cerebral palsy
(7) Poutney, Mandy, Green and Gard, 2009 – Hip subluxation and dislocation in cerebral palsy
(8) Hankinson and Morton, 2002 – Use of a lying hip abduction system in children with bilateral cerebral palsy
*Under supervision following a proper clinical and risk.
Prepared in conjunction with the team at Jenx UK.









