In 2013 Hounslow wheelchair service (WCS) won a Dragons’ Den style competition within Hounslow Community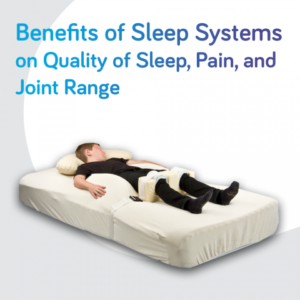 Healthcare (HRCH) Trust. The bid was for funding for a pilot study researching sleep systems as part of a twenty four hour postural management programme. Consideration of twenty four hour postural management and provision of sleep systems was patchy within the trust. The pilot study consisted of four participants over a period of six months. Evidence for joint range, quality of sleep, quality of life, pain, and goal attainment scaling (GAS) outcomes, were gathered at baseline, with data then being collected at monthly intervals. The outcomes have been positive, with sleep quality having improved, quality of life for both parents and participants having improved, and GAS outcomes having been met and exceeded.
Healthcare (HRCH) Trust. The bid was for funding for a pilot study researching sleep systems as part of a twenty four hour postural management programme. Consideration of twenty four hour postural management and provision of sleep systems was patchy within the trust. The pilot study consisted of four participants over a period of six months. Evidence for joint range, quality of sleep, quality of life, pain, and goal attainment scaling (GAS) outcomes, were gathered at baseline, with data then being collected at monthly intervals. The outcomes have been positive, with sleep quality having improved, quality of life for both parents and participants having improved, and GAS outcomes having been met and exceeded.
We found that there is little research evidence for clinicians to support provision and funding of sleep systems. Our aim was to obtain evidence of the clinical and quality of life effects of sleep systems for service users and carers. Also to ascertain any associated cost savings that had been made in our participants’ overall care. Our objective was to expand the remit of Hounslow WCS and establish a Twenty Four Hour Postural Management Service. The information gathered from the pilot study would inform us how to deliver the service, budget requirements, and assist with building a business case to present to commissioners.
The aim was to build on the evidence that has already been collected through previous research by building on their methods. A Mac Keith multidisciplinary meeting formulated a consensus statement concerning postural management for children with cerebral palsy: ‘Children in GMFCS groups 4-5 should start twenty four postural management programmes in lying as soon as appropriate after birth, in sitting from 6 months and in standing from 12 months.’ Both Terry Pountney (Pountney et al, 2009) and Ginny Humphreys (Humphreys, 2010) have conducted research which also supports the use of sleep systems.
Materials and Methods: In January 2014 we began a pilot study to measure the effect of the sleep systems. The four participants were aged between 3 and 21. We used the Chailey sleep questionnaire for the assessments and for the ongoing reviews to record changes in sleep quality, posture and use of the system. Sleep quality was also recorded using the Chailey sleep diaries. To assess quality of life for the family and the participant we used GAS. Pain levels were measured using the paediatric pain profile; postural assessment using the Oxford Centre for Enablement forms, and the neutral zero method was used to record joint range.
Having reviewed the sleep systems available we chose the Symmetrisleep system. This had a wide variety of options, could be used on any bed and could be transported with ease as many of our service users travelled abroad. The ideal was to use one system to limit variability in the results but, where this could not meet the participants’ needs, alternatives would be considered.
The study is still ongoing although preliminary results are positive. One participant was waking every 40 minutes to 2 hours and he is now only waking once during the night. The sleep system is now managing his posture at night and his tone has reduced. Another participant was waking regularly throughout the night as she would extend and scissor her legs which would cause discomfort. Her posture is now maintained and she is sleeping through the night. Her parents have also noted that her arms, which used to be held in flex ion, are more relaxed and extended. Both parents have reported that they are feeling more refreshed as they have uninterrupted sleep. In one case the whole family sleep in one room and so this has improved all their sleep. All have reported that their GAS outcome measures have been met or exceeded. All participants’ joint ranges have been maintained, and their pain has not increased, even, in some cases, decreased.
The Chailey sleep questionnaire and sleep diaries have been invaluable in recording the level of detail required for prescription.
The borough has a very diverse population. Clear pictorial user guidelines have been critical, as some of the participants have English as their second language. The clear guidelines have meant the systems have been used correctly and consistently.
Another crucial aspect is that we have given the families close support. Two weeks after provision, a visit is made to assist the families and then once a month. In some cases we have been there for emotional support; some families have been, and still are, struggling, and we are there to help ease some of their carer burden. By visiting regularly this has also enabled us to react quickly where improvements need to be made, and we have been able to see how rapidly changes in sleep quality have occurred. In rolling out the project we will need to ensure that we have the staffing to enable us to give our families support to ensure the success of the systems.
The study has helped us to establish service delivery and budget requirements. Our trust is supporting us in funding this for another year. We are writing a business case which is being presented to our commissioners to become a Twenty Four Hour Postural Management Service. In recognition of our work our trust nominated us for a Health Service Journal award in the Compassion in Care category; we were then shortlisted as finalists.
Humphreys, G., (2010). Posture and Sleep in Children with Cerebral Palsy. PhD Thesis.
Pountney, T.E ., Mandy, A., Green, E., Gard, P.R. (2009). Hip subluxation and dislocation in cerebral palsy – a prospective study on the effectiveness of postural management programmes. Physiother Res Int., 14( 2), 116-127







