All information contained in this document is provided to overview the equipment available for children with Cerebral Palsy (CP). Whilst there are different options discussed in this PDF, every postural support device used for any child should be assessed by a qualified therapist with knowledge of the child’s condition and unique circumstances.
What is Cerebral Palsy (CP)?
- Celebral Palsy is the most common physical disability in childhood, it is said to affect an estimated 17 million people worldwide (1).
- Cerebral Palsy an umbrella term that covers a group of disorders, it is permanent and caused by a combination of events that result in damage to the developing brain. Whilst CP is not a progressive condition, its presentation can be (2).
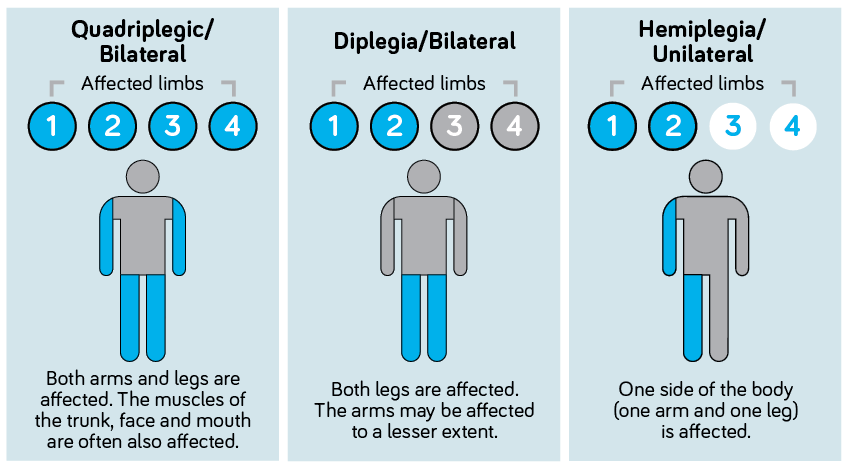
CP can be described by the area/s of the body that is affected:
Quadriplegic CP: Where all four limbs of the body are affected, there is also involvement of the muscles of the trunk, head, and neck, including the face and mouth.
Diplegic CP: Where both legs are affected. The arms may also be affected but to a lesser extent.
Hemiplegic CP: Where one side of the body is affected, left or right, involving both arm and leg.
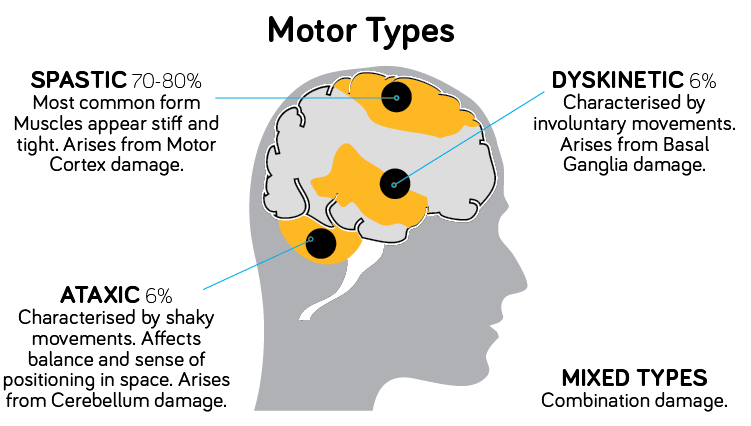 CP can also be described by the area of the brain which is affected, this indicates how a child’s movement is likely to present (3):
CP can also be described by the area of the brain which is affected, this indicates how a child’s movement is likely to present (3):
Spastic CP: this refers to damage to the area of the brain called the motor cortex. This is the most common type of CP and is characterised by increased muscle tone and stiffness in the muscles of the affected body region.
Dyskinetic CP: this refers to damage of the Basal Ganglia which results in involuntary movements which are out of the child’s control.
Ataxic CP: this refers to damage of the Cerebellum, it is characterised by shaky or poorly controlled movement, it can also have a significant impact on balance and proprioception (sense of positioning in space).
Mixed CP: this refers to a combination of the above types due to damage of multiple parts of the brain.
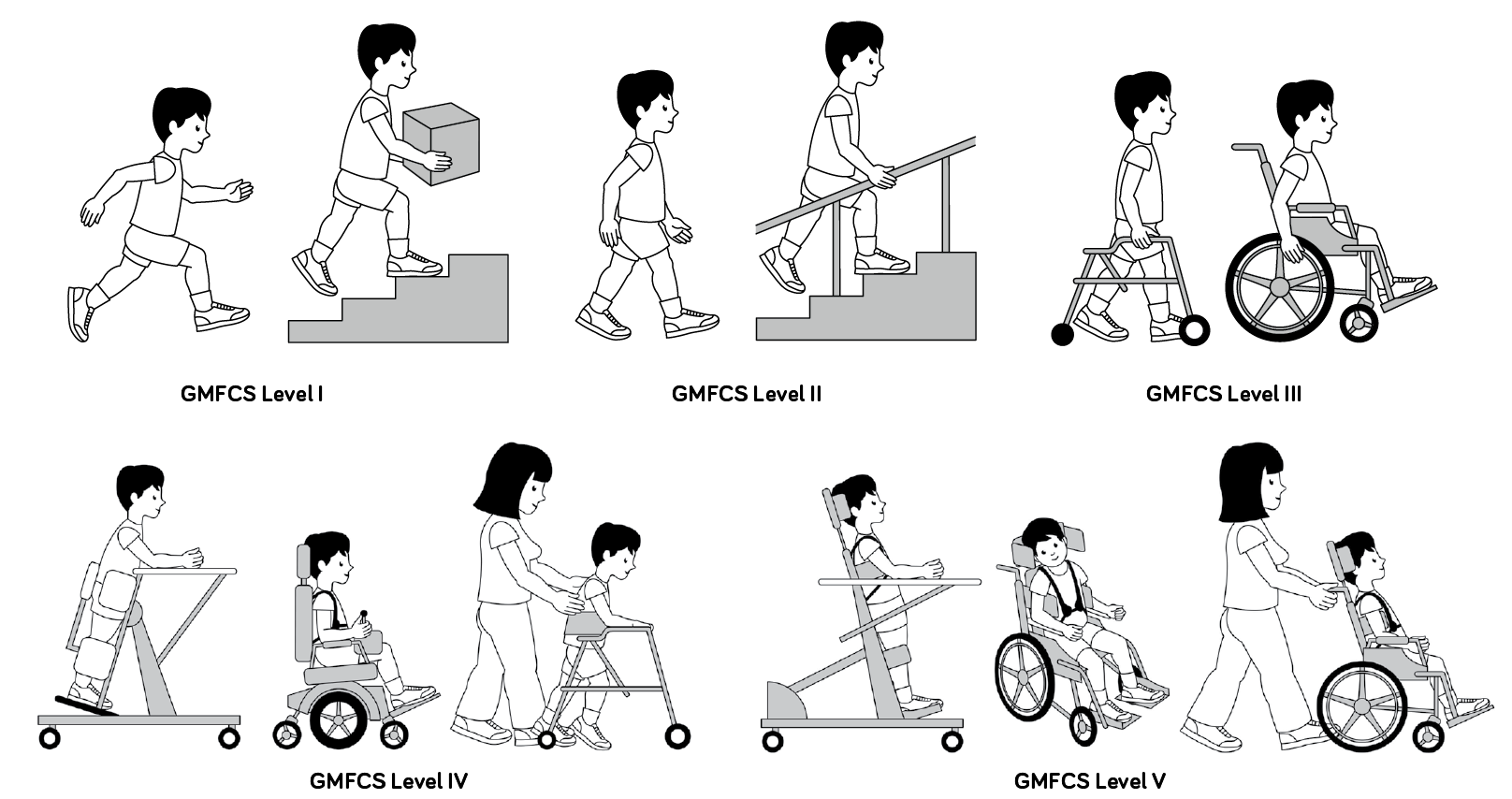
The Gross Motor Function Classification Scale (GMFCS) refers to how the gross motor skills of a child or young person are affected.
Other classifications include:
- The Manual Ability Classification System (MACS) – fine motor skills
- The Communication Function Classification System (CFCS) – communication.
The GMFCS is useful in providing a clear description of a child’s motor function. This in turn outlines the assistive technology (AT) they will likely need to support them, now and in the future. The GMFCS ranges from level I to V, where a child is classified as level III – V it is likely they will require assistive devices for mobility and postural support, although a child of any level may require some form of AT. Importantly, the mode of support required may be different depending on the setting the child is in, whether at home, school or in the community.
Gross Motor Skills
The gross motor skills (eg. sitting and walking) of children and young people with cerebral palsy can be categorised into 5 different levels using a tool called the Gross Motor Function Classification System (GMFCS) developed by CanChild in Canada.
GMFCS Illustrations 6-12: © Bill Reid, Kate Willoughby, Adrienne Harvey and Kerr Graham, The Royal Children’s Hospital Melbourne
- CP affects the motor function of a child which can create a significant risk for the development of body shape changes and asymmetrical postures. As GMFCS levels increase, so too does the likelihood of asymmetry and associated pain (4). Prolonged time spent in unsupported positions, compounded by the effects of gravity, contribute heavily to these changes in body shape. Over time this can lead to fixed postures, resulting in difficulties relating to function, comfort and health (5).
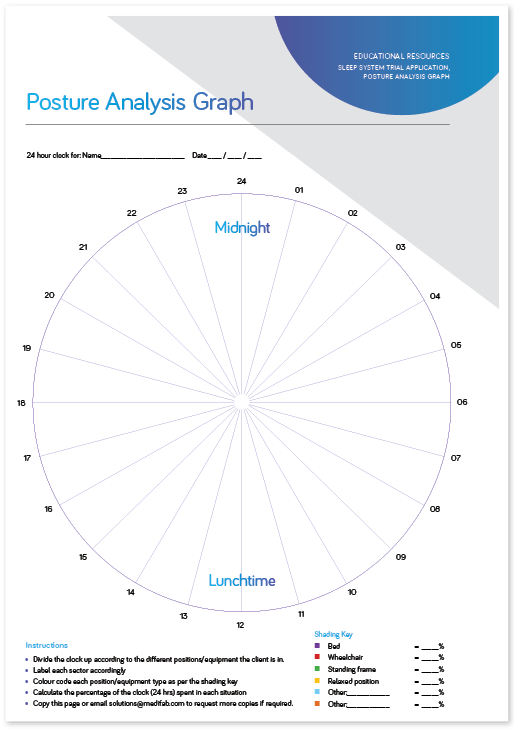
- 24-hour postural care is an approach which assesses all positions that a child uses throughout the day and night. Taking this approach for children with CP is important for the protection of body shape and promotion of health and function. The positions of lying, sitting and standing should form the basis for this 24-hour approach.
- If you are considering the 24 hour postural care approach for a child you work with, our posture analysis graph is available to support your assessment, encouraging parents and caregivers to break down how much time a child spends in different positions across 24 hours of the day.
- How this approach looks for each child will be different. Comprehensive assessment, along with co- production with families and care givers, is necessary to achieve the best outcome for the child. As children grow and their function and movement change, it is important that plans are reviewed regularly to ensure children remain supported. When introducing a new piece of equipment, or when changing posture through existing equipment, we must be gentle and be considerate of comfort. Tolerance of new, more symmetrical positions will need to be built and developed over time.
- CP and its secondary complications will affect the body 24 hours a day. Considering how a child sleeps, and what support they need in lying, is as important as any other position they adopt during the day.
- Common postural and body shape changes experienced by children and adults with CP can often be linked to the unsupported and asymmetrical positions assumed in lying. Over time the combination of asymmetrical positioning and gravity will cause body shape change to occur. This will impact significantly on what the child can do during the day, how functional they are, and ultimately their quality of life (5).
- Pelvic obliquity, pelvic rotation, windswept hip deformity, and scoliosis are all commonly seen in children and adults with moderate to severe CP, all can be linked to unsupported and asymmetrical side-lying.
- Chest shape and rib cage deformity can be seen as a direct result of unsupported lying in any position, even in supine.
- Anterior pelvic tilt, lumbar lordosis, and upper limb contractures that impact function are also commonly linked with prone sleeping.
- As GMFCS level is indicative of motor function, this allows identification of those less able to change their position independently. Children at GMFCS level IV and V are less able or unable to change their position in lying. As a result, they spend prolonged periods of time in one position during the night (6). If unsupported, the likelihood that this position will be asymmetrical is high and over prolonged periods of time will become destructive (5). Preventative and proactive approaches for providing supported positions for these children should be taken to avoid these changes from occurring in the first place.
- If a child is using moderate or complex seating to meet their postural needs during the day, they require assessment for support at night-time. Equally if achieving a comfortable and symmetrical seated position is becoming harder, how the child is lying at night should also be considered and reviewed.
- If you are considering an assessment of a child’s night-time positioning needs, our “Pre-assessment Form for Night-time Positioning Equipment” is available to facilitate the decision-making process.
- Some children with more movement control utilise independent position changes at night for the function of a good night sleep. Appropriate rest is intrinsically linked with overall health and therefore it is vital that support used at night-time does not disturb this very important function.
- Children with CP may adopt seated positions for large periods of their day, often with different seating systems prioritised for different activities or functions. The degree to which a child’s CP impacts their postural control in sitting can vary greatly depending on multiple factors such as; impairment to head control, sitting balance & and upper limb function. Whilst some children with CP will require no additional support in sitting, those who are GMFCS III and above are likely to need some support, increasing to significant support for children who are GMFCS level V. Achieving stable and functional seated positions with a child across their day provides them with the opportunity to communicate, engage with their environment, play, have fun and so much more. Appropriate postural management in sitting can therefore make up a large part of a child’s day and be very effective in improving or maintaining their body shape and function.
- When considering the postural support requirements in sitting it is also important to consider the functional goals and requirements for a particular chair and how that relates to the environment it’s being used in.
- Different sitting positions and the support needed in these positions will be varied across a child’s day:
- Support in a mobility device allows the child to be in a functional position to engage in active mobility, driving controls for powered mobility, or for safe and comfortable seating so that they can be transported by family or carers
- A supportive indoor seating system provides a functional surface that can be used at home, at school, at day program, or any other indoor setting for play, activity, and fun. Full support of the trunk and pelvis to optimise head and upper limb control, along with unique postural supports, provides a seating system more geared towards activities than mobility. Most of these chairs have an option for a Hi-lo base which allows for improved access to different levels of the environment for socialisation, learning, transfers, and inclusion into family time.
- 1 in 10 children with CP have severe vision impairment. Having optional accessories to support the use of sensory toys can be a fantastic way to facilitate play that meets the needs of the child (2).
- Children with CP often have issues with continence and constipation, 1 in 4 have bladder control problems (7). In addition, postural support needs add complexity to providing opportunity for toileting, showering, and bathing, and can add significant time to these activities. Access to supported sitting for the time in the bathroom is crucial to allow children and their parents/carers access to comfortable, safe, and supported care time together. The bathroom is also a slippery environment for everyone, even more so for those with reduced motor function or control. It is therefore also important that a solution provided to support children in this environment is mobile as to maintain safety and avoid accidents.
- Accessing transport for children with CP can be challenging, but every child has a right to be safe and supported on the road or in the air. If a mobility device has the appropriate features and certification, a child can be transported safely within it, provided it is secured within a compliant vehicle. When a child does not have access to this type of vehicle, particularly younger children where a diagnosis may be new, or where the transition to a modified vehicle is not appropriate, then a special purpose car restraint is the best option to provide this safe and supported position. Some of these options provide the compatibility to also be used on an aircraft. Restraint may be the best option, providing support for travel not only helps maintain symmetry & comfort, but also ensures the child is in the safest position possible for safety devices such as seatbelts to do their job properly.
- Changing requirements and functions within different seats may result in children with CP becoming more fatigued thus increasing their postural support needs. Children with CP are likely to experience periods of the day where they need more or less postural support. The requirement on the seating surface will therefore change throughout the day and will often be related to the tasks they are performing. Ability to manage this through changing the base of support with tilt for a more supported and less energy expensive position is crucial. Likewise, when more activity is on the cards, a more upright position may be required.
- A child’s movement and motor function in standing and walking are also likely to be impacted by their CP, even if very minimally. As shown earlier in this blog, the effect on motor function is classified using a 5-level system. Typically, those who are level III+ will require assistance with walking and standing.

- Due to the impact on motor function, children with CP can experience delays in reaching developmental milestones associated with standing. Research tells us it is important that children are supported in standing from the developmentally appropriate age of 9-12 months (8). Supporting a child into standing at this time can ensure they receive the benefits of weight-bearing and being upright. It is understood that without the loading of the hip joint in this early age, children are at much higher risk of developing disorders relating to their hips (8).
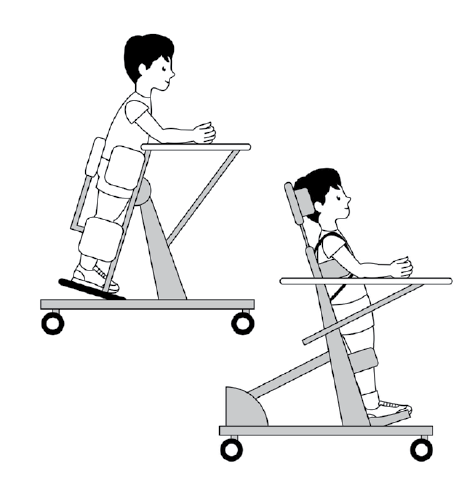
- Standing frames are pieces of equipment that support a child in standing, using the necessary postural supports to keep them in a safe and functional position. When considering which type of standing frame is best for a child with CP, it is important to consider the postural control they have, their current GMFCS level, and the likelihood for the development of skills in the future.
- As a rule of thumb, children with GMFCS level V will have reduced or no head control, and whilst this may not be permanent, it is a good indicator that a supine supportive standing frame will be the best option for these children. For children at lower GMFCS levels who have some amount of head control, a prone or upright stander may be more appropriate.
- Abduction in standing can also be considered for children with CP. Abduction helps to provide a stretch to the adductor muscles, improve hip joint alignment, increase weight-bearing for some children and provide a position to maintain range of movement at the hip (8,9).
- It is important to match the level of support in a standing frame to the level of support the child requires, especially in early intervention standers. As children’s motor skills are constantly developing at this early age, a standing frame that provides opportunity to support this development through appropriate levels of support is paramount.
- There are multiple factors to consider when prescribing a standing frame, including when a standing program may be unsafe to start or continue with. To facilitate assessments for standing frames check out our Standing Assessment Tool used to assist with the prescription process.
- It is important to note that as a child with CP continues to develop their motor skills the support they require for standing will also change. Just because a child starts with using standing frames does not mean they will always have to use one. Early intervention standing frames, in particular, may offer flexibility to change from supine to prone configuration as a child’s skills develop.
- As children with CP progress with their motor function, they may begin to develop skills in dynamic standing and walking. As this progress and development occurs, it is important to consider a standing frame that can be easily adjusted to challenge users at times and supports them at others. Having brief and supervised time with less support in a standing frame can be an effective strategy to promote skill development and postural control. Where progress into dynamic weight-bearing occurs, the potential for independent mobility is greatly increased regardless of whether the child requires equipment to do so. As this provides independence, it is rightly prioritised in therapy and goal setting as a way of improving function to the greatest benefit. Initially, time spent in weight-bearing during the acquisition of this skill may be low and infrequent, increasing as stability and control are established. During this process, the use of standing frames can be continued as a way of ensuring prolonged experiences of being upright and weight-bearing.
- Alliance, C., 2022. What is cerebral palsy? | Cerebral Palsy Alliance. [online] Cerebralpalsy.org.au. Available at: <https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-c… [Accessed 8 February 2022].
- Alliance, C., 2022. Facts about cerebral palsy | Cerebral Palsy Alliance. [online] Cerebralpalsy.org.au. Available at: <https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-c… [Accessed 8 February 2022].
- Alliance, C., 2022. Types of cerebral palsy | Cerebral Palsy Alliance. [online] Cerebralpalsy.org.au. Available at: <https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-c… [Accessed 8 February 2022].
- Casey, J, Rosenblad, A & Rodby-Bousquet, E 2020 ‘Postural asymmetries, pain, and ability to change position of children with CP in sitting and supine: a cross sectional study’, Disability and Rehabilitation
- Hills, S & Goldsmith, G 2010 ‘Biomechanics and prevention of body shape distortion. Tizard Learning Disability Review
- Sato, H 2020, ‘Postural deformity in children with CP: Why it occurs and how it is managed’, Physical Therapy Research
- Alliance, C., 2022. How does cerebral palsy affect people? | Cerebral Palsy Alliance. [online] Cerebralpalsy.org.au. Available at: <https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-c… [Accessed 8 February 2022].
- Paleg GS, Smith BA, Glickman LB 2013. Systematic review and evidence-based clinical recommendations for dosing of pediatric supported standing programs. Pediatr Phys Ther
- Martinsson C, Himmelmann K 2021. Abducted Standing in Children With Cerebral Palsy: Effects on Hip Development After 7 Years. Pediatr Phys Ther. https://journals.lww.com/pedpt/Abstract/2021/04000/Abducted_Standing_in_…





