Benefits of standing in Abduction: Early Intervention through to Active Teens
There is a great deal of research that supports the improvement of bone mineral density, reduction of spasticity and maintaining hamstring length. One of the most prevalent problems for children with cerebral palsy with a GMFCS 3 or above is the malformation of their hip joints. When we are born, our acetabulum (hip socket) is not yet formed. It is the process of being in an upright standing position, bearing weight through our hips, knees and feet, as well as being mobile that helps to form healthy hip joints. By accepting force through the pelvis, our acetabulum forms over time. At a young age a child’s bones are growing and malleable. It isn’t until around 6-8 years old their bones harden and joints are less pliable to mould into their ‘typical’ shapes. Therefore, hip development is one of the main reasons to adopt a standing program at an early age. The evidence suggests that a child who is up and standing by the age of around 12 months is more likely to develop healthy hip joints and reduces the risk of hip subluxation (Paleg 2013).
But is there anything else we can do to help aid this process and increase the likelihood of forming ‘normal’ hip joints?
Standing in abduction has been found to have a number of benefits to the musculoskeletal system. A study published from Sweden in 2011 describes a randomised controlled clinical trial involving 80 children. This study looked at the efficacy of standing children with Cerebral Palsy in abduction whilst weight bearing. To summarise the conclusion they found that ‘ Straddled weight-bearing, 1 hour per day, may reduce the MP after adductor-iliopsoas-tenotomies or prevent an MP (Hip Migration Percentage) increase and preserve muscle length in children with cerebral palsy who did not need surgery’ (Martinsson 2011). By reducing a child’s Hip Migration percentage, effectively you are lowering the risks of subluxation and dislocation, which often results in costly and painful surgical intervention. If we simplify that further, by locating the head of the femur in a more exaggerated angle, children with Cerebral Palsy are more likely to have healthier hip joints.
Another study published in 2015 from Barcelona reviewed the progress of children with Spastic Cerebral Palsy who were stood in Abduction from the ages of 12-14 months through to 5 years old. The children were stood in abduction with 10 degree’s less than their maximum ability, which averaged out to be around 30 degrees on each limb. This study had a number of positive findings, including a significant reduction in Hip Migration Percentage. They also found that the children had increased hip stability, no requirement for hip corrective surgery and none of the children performed a scissoring gait pattern. There was also a notable reduction in spasticity as well as the maintenance of adductor and hamstring lengths (Macias-Merlo L, 2015). We could surmise from these findings that not only the children’s skeletal health was vastly improved; it contributed to preventing the need for surgical intervention. The fact that these children had a more efficient and ‘normal’ gait pattern would likely contribute to their overall mobility, independence, general health and inclusion.
Focusing on only these 2 studies there does appear to be a number of clinical reasons why we would stand a child from an early age in abduction. However, what about slightly older children and teenagers? Do they still benefit from standing in abduction?
It could be argued that it is highly important to continue an abduction standing programme as long as the child/adult can maintain this approach. Looking at the research we know that standing in abduction can:
- Reduce Spasticity
- Help to reduce Hip Migration
- Maintain Adductor & Hamstring length
- Reduces/prevents a scissor gait pattern
No matter how old a person is, these outcomes can greatly improve someone’s physical and mental health, and increase their quality of life. This coupled with the more general benefits of adopting any upright standing programme:
- Increased bone mineral density
- Better functioning bodily systems
- Increased body & spacial awareness
All of which contribute to holistic approach of postural and physical management, helping to prevent or minimise the development of secondary complications for a person with disabilities.

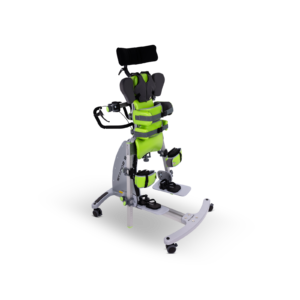
Continuing with the core principals of clinically correct positioning, Standz size 2 allows for clinicians to support older children and adolescents as they move from postural development through to postural maintenance.
More than just a scaled up version of the original Standz, size 2 offers function and accessories that are appropriate for an older, taller, heavier and stronger user whilst keeping the much loved simplicity of adjustment and use found on the original Standz.
- Considerations related to weight-baring programs in children with developmental disabilities. (Sturberg WA. 1992)
- Hip subluxation and dislocation with postural management. (Pountney T . Et al, 2009)
- Hip and spine in children with cerebral palsy: musculoskeletal development and clinical implications (Gudjonsdottir BSV 1997)
- Effects of the standing program with hip abduction on hip acetabular development in children with spastic diplegia (Macias-Merlo L, et al. 2015)
- The effects of weight-bearing in Abduction and Extension on hip stability in Children with cerebral palsy (Martinsson C, et al. 2011)
- Severe and Complex Neurological Disability: Management of the physical condition. (Pope P. et al 2007)
- Systematic Review and Evidence-Based Clinical Recommendations for Dosing of Paediatric Supported Standing Programs (Paleg, Ginny, S et al 2013)