This blog aims to provide some guidance on the potential causes and presentation of tight hip flexors for wheelchair users. Seating solutions will be considered along with how Spex cushions can help to manage outcomes for functional seating. Individuals with tight or hypertonic hip flexors may sit in anterior pelvic tilt (an anteriorly tilted pelvis). This exaggerates the lumbar lordosis of the spinal column (Mansfield & Neumann, 2019). When seated, these individuals will lean forward and may need to prop on the arm supports of the wheelchair or their thighs (Lange & Minkel, 2018) which can affect alignment and function during activities performed in the wheelchair.
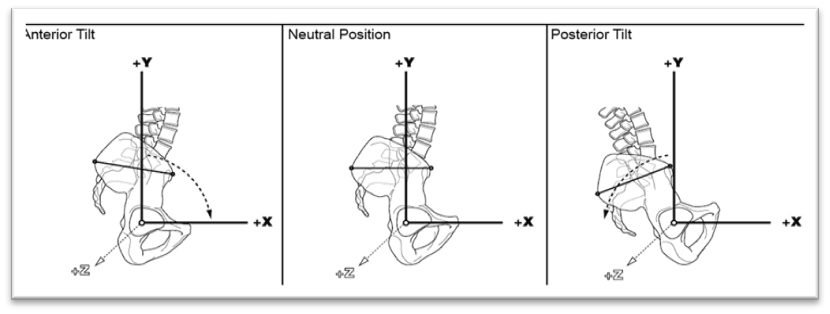
Anterior Pelvic Tilt (left) where anterior superior iliac spine (ASIS) is lower than the posterior superior iliac spine (PSIS) and the pelvis has rotated forward (Waugh & Crane, 2013)
What are the hip flexors?
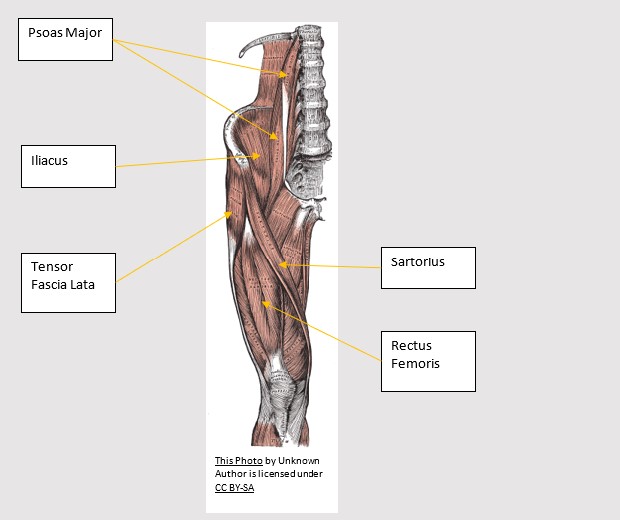
The hip flexors include several muscles, which originate on the pelvis, spine or sacrum and insert onto the lower limb. The abdominal muscles provide stability when the hip flexors are working and mobilising – without this, the pelvis can be pulled into anterior pelvic tilt when, for example, lifting the knee. The hip flexors are also under constant tension and can become shortened or tight because of habitual postural positioning which can then also create an anteriorly tilted pelvis and exaggerated lumbar lordosis (Simancek, 2013). We might see this more so during standing or lying when the hips are fully extended and the trunk upright. Tight hip flexors in sitting may affect the ability for the person to sit with their pelvis held in neutral tilt whilst the legs are resting on a horizontal surface, instead pulling the pelvis forward into anterior tilt.
The primary hip flecors include the following muscles (Gerhard et al., 2011):
- Rectus femoris (a bi-articular muscle that traverses both hip and knee, with greater power when the knee is flexed, and it is ‘stretched’)
- Illiacus & Psoas (these are often referred to ‘iliopsoas’ but remian, in face, two muscles)
- Illocapsularis, and
- Sartorius
| Muscle | Origin | Insertion | Action | Considerations During Muscle Testing |
|---|---|---|---|---|
| PSOAS MAJOR | L1-L5 vertebrae (transverse processes)
T12-L5 vertebral bodies |
Femur (lesser trochanter) | Hip flexion | Substitution by other hip flexors, in event of weakness of iliopsoas, can result in either abduction and external rotation (sartorius) or abduction and interanl rotation (tensor fascia lata) |
| ILIACUS | Iliac fossa (anterior 2/3) | Femur (lesser trochanter) | Substitution by other hip flexors, in event of weakness of iliopsoas, can result in either abduction and external rotation (sartorius) or abduction and interanl rotation (tensor fascia lata) | |
| SARTORIUS | Illium (anterior superior spine) | Tibia (medical surface) | Hip flexion abduction & external rotation | Substitution by other hip flexors, in event of weakness of iliopsoas, can result in either abduction and external rotation (sartorius) or abduction and interanl rotation (tensor fascia lata) |
| ILIOCAPSULARIS | Anterior-inferior iliac spine (AIIS) and anterior hip capsule | Distal to the lesser trochanter | Hip stabiliser and synergistic to iliacus. | Atrophy can result in impingement and reduced hip stability |
| RECTUS FEMORIS | Anterior-inferior iliac spine (AIIS) and superior to acetabulum. | Base of the Patella | Hip flexion | One of the four quadriceps muscles and direct antagonist to the hamstrings. |
What can contribute to tight hip flexors?
- Adaptive shortening can occur in the hip flexors due to prolonged sitting postures or lying with the knees drawn up towards the chest (for example when lying on your side). This can lead to tightness and discomfort when moving into a standing position.
- Hip flexion contractures are associated with hip dysfunction. Osteoarthritis, trauma and associated pain and protective guarding in response to this can lead to contractures through shortening of iliacus, psoas major, rectus femoris or anterior hip capsule (Fagerson et al., 2016).
- Spasticity related to neurological conditions that may present as “increased tone, clonus, spasms, spastic dystonia and co-contractions” (Kheder & Nair, 2012)
- Existing spasticity can also be triggered by discomfort related to, for example, hip pain, pressure injuries, constipation, or urinary urgency.
What should we do to optimise posture in wheelchair sitting?
The key to management of tight hip flexors is accurate assessment and understanding what the triggers may be for increased hip flexion in a seated position, medical condition, and pain limits and whether the associated anterior pelvic tilt is reducible or non-reducible. It is important that we consider the biomechanics of the body in sitting. A flat cushion may increase the thigh to trunk angle and hip flexion angle in relation to a neutral pelvis. This can contribute to instability, and reduced pressure distribution and relief.
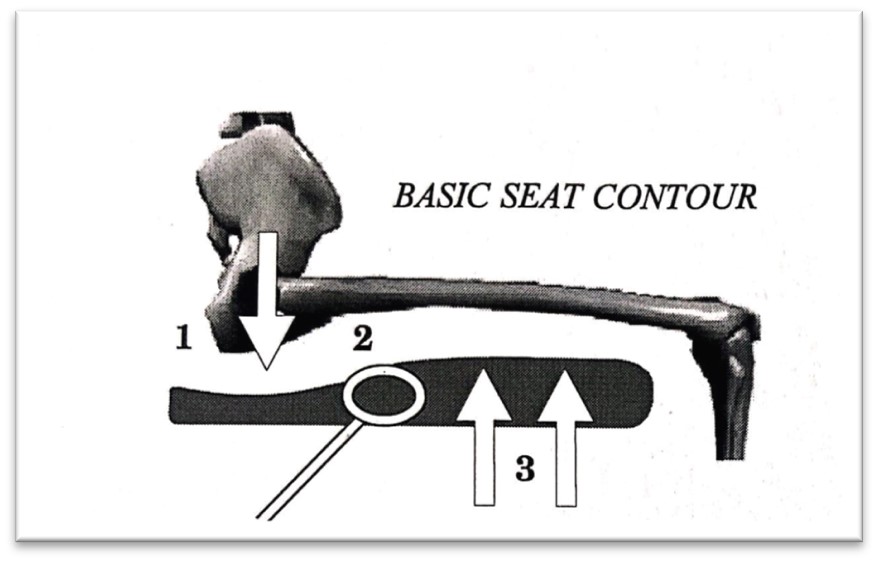
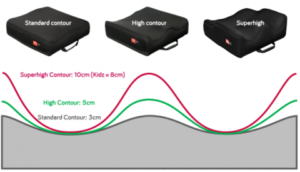
A basic seat cushion contour should be slightly lower under the pelvis, there should be an uphill section or pre-ischial shelf to stop the pelvis sliding forward and finally, a higher component under the thighs for effective leg support. (Engström, 2011)
Reducible anterior tilt and hip flexion tightness presentation:
Any intervention to reduce hip flexion and anterior pelvic tilt should be within pain limits and may therefore need a gradual approach dependent on the needs of the wheelchair user. A priority should be placed on reorientating the pelvis into a neutral alignment with ASIS and PSIS level. This can be achieved by providing an anterior pelvic belt at the level of the anterior superior iliac spine (ASIS) to block or reduce the degree of anterior tilt. This, in turn, can reduce the associated exaggerated lumbar lordosis created by the anterior pelvic tilt and ensure optimal alignment of the trunk and head above the pelvis.
Additional considerations include:
- If reducing anterior pelvic tilt creates pain in the hip due to the tight/shortened hip flexors, then the cushion may need to accommodate the hip flexion angle by providing some ramping under the thighs so that the knees are higher than the level of the hip with the option to reduce this ramping over time.
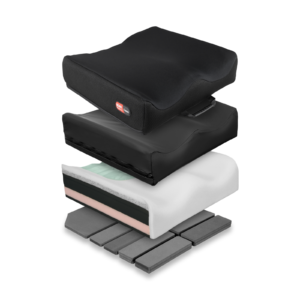
- Additional contouring to the supporting cushion surface around the pelvis and thighs to assist with pressure distribution and provision of stability to optimise relaxation and reducing triggered tight hip flexors. Consider the cushion configuration as it relates to pressure management by selecting materials which allow immersion, envelopment, and thermoregulation.
- Also consider the back and lateral or anterior trunk supports to provide reinforcing support in the presence of weak abdominal muscles or spasticity.
- A tray and angle adjustable arm supports may be required to provide additional stability, support and ultimately, function
 |
 |
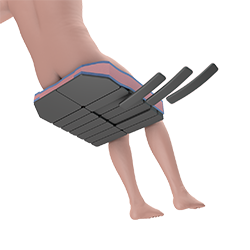 |
Spex Classic cushion: varying foam configurations (left) and contouring (centre) allow for comfort and pressure management, and can allow for hip flexion responsiveness through configuration of the underlying pocket-layer (right)

Spex cushion foam selections available as taken from the Build-your-own cushion script form
Gravity can also be harnessed as a ‘friend’, providing that the cushion, back and lateral trunk supports optimise acceptance of the supports, stability and reduce the effort of sitting for the wheelchair user. whilst maintaining the line of gravity within the base of support. When thinking of the sagittal plane movements (flexion/extension), if the trunk and pelvis is neutral (upright) and the line of gravity is within the base of support, then gravity is less likely to influence secondary postural distortion development, whilst still affecting a downward force on the thighs towards a more neutral hip position for sitting. This can support gradual reduction of the tight hip flexors. In this way an adjustable or contourable cushion can allow easy reconfiguration to respond to improved hip alignment in sitting.
 |
 |
Contourable cushions that allow for hip flexion beyond 90° in sitting include the Spex Flex Cushion – 70-110° hip flexion range (left) and Spex cushion – 85-95° hip flexion range(right) and careful consideration should be given to the back and trunk supports to optimise contact and stability.
Non-reducible anterior pelvic tilt and hip flexion presentation:
In addition to the cushion configuration considerations (above), the following will help improve sitting stability:
- Anterior pelvic support belt at the level of the ASIS to block further anterior tilt and provide stability.
- Ramping the cushion (front higher than the back) to bring the pelvis more into a neutral alignment.
- In the presence of an exaggerated lumbar lordosis, ensure that the user maintains contact with the back support and that back support contours provide upward reinforced support to the weight of the trunk.
- A tray or adjustable arm rests should be considered for additional lateral and anterior stability during siting.
A comprehensive clinical assessment will inform interventions needed for postural reinforcement and reduction of distortions, but please do not forget that seated mobility should be functional and therefore needs to consider both reducing the effort of sitting and optimising functional activity within the wheelchair.
Seating provision should always be functional, meaning that it is an “individually driven, guide-based seating intervention to promote task performance
– Costigan & Light, 2011
Thank you for reading!
- Babst, D., Steppacher, S. D., Ganz, R., Siebenrock, K. A., & Tannast, M. (2011). The iliocapsularis muscle: an important stabilizer in the dysplastic hip. Clinical orthopaedics and related research, 469(6), 1728–1734. https://doi.org/10.1007/s11999-010-1705-x
- Costigan, F. A., & Light, J. (2011). Functional Seating for School-Age Children with Cerebral Palsy: An Evidence-Based Tutorial. Language Speech and Hearing Services in Schools, 42(2), 223. https://doi.org/10.1044/0161-1461(2010/10-0001)
- Engström, B. (2011). ERGONOMIC SEATING. A True Challenge. Wheelchair Seating & Mobility Principles (2nd ed.). Engstrom Concepts AB.
- Fagerson, T. L., Babatunde, O. M., & Safran, M. R. (2016). Chapter 18 – Hip Pathologies: Diagnosis and Intervention. In D. J. Magee, J. E. Zachazewski, W. S. Quillen, & R. C. Manske (Eds.), Pathology and Intervention in Musculoskeletal Rehabilitation (Second Edition) (pp. 651–691). W.B. Saunders. https://doi.org/10.1016/B978-0-323-31072-7.00018-X
- Gerhardt, M. B., Logishetty, K., Meftah, M., & Ranawat, A. S. (2011). CHAPTER 2—Arthroscopic and Open Anatomy of the Hip. In J. K. Sekiya, M. R. Safran, A. S. Ranawat, & M. Leunig (Eds.), Techniques in Hip Arthroscopy and Joint Preservation Surgery (pp. 9–22). W.B. Saunders. https://doi.org/10.1016/B978-1-4160-5642-3.00002-5
- Kheder, A., & Nair, K. P. S. (2012). Spasticity: Pathophysiology, evaluation and management. Practical Neurology, 12(5), 289–298. https://doi.org/10.1136/practneurol-2011-000155
- Lange, M. L., & Minkel, J. L. (2018). Seating and Wheeled Mobility: A clinical resource guide. Slack Incorporated.
- Mansfield, P. J., & Nemann, D. A. (2019). Chapter 9—Structure and function of the hip. In Essentials of Kinesiology for the Physical Therapist Assistant (pp. 233–277). Elsevier. https://doi.org/10.1016/C2016-0-03960-8
- Simancek, J. A. (Ed.). (2013). Chapter 9—Hips and Thighs. In Deep Tissue Massage Treatment (Second Edition) (pp. 134–157). Mosby. https://doi.org/10.1016/B978-0-323-07759-0.00032-8
- Waugh, K., & Crane, B. (2013). A clinical application guide to standardized wheelchair seating measure of the body and seating support surfaces. (Revised). Assistive Technology Partners. https://pva-cdnendpoint.azureedge.net/prod/libraries/media/pva/library/publications/lib_waugh-guide-to-seating-v2-measures-revised-ed-compressed.pdf




