This activity toolkit has been developed to educate therapists, carers and children with disability on the World Health Organisation and UK Chief Medical Officer physical activity guidelines for disabled children and adolescents, as well as the concept of 24 hour movement principles for optimal health.
The toolkit is intended be a resource for adapting guidelines to the unique movement abilities of children or teenagers with any type of disability, with some additional information for early years.
In the PDF format of this toolkit, all links in the resource sections are clickable hyperlinks intended to provide support to get more active, improve sleep, and link to worldwide guidelines and charity organisations for funding.
This toolkit has been greatly inspired by the brilliant work at the Canadian Disability Participation Project:

CHILDREN AND ADOLESCENTS
(aged 5–17 years)
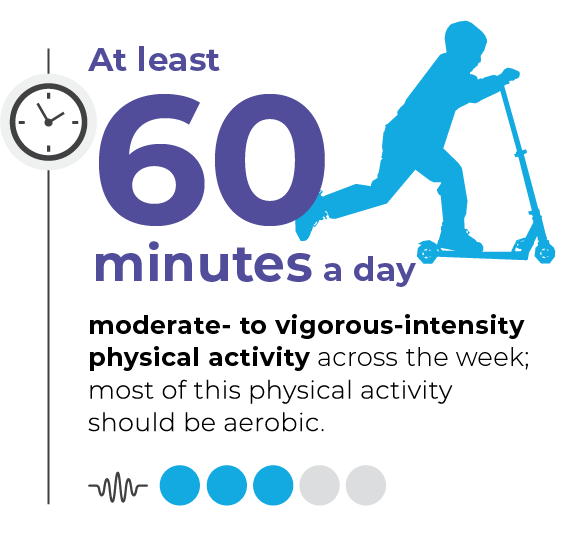
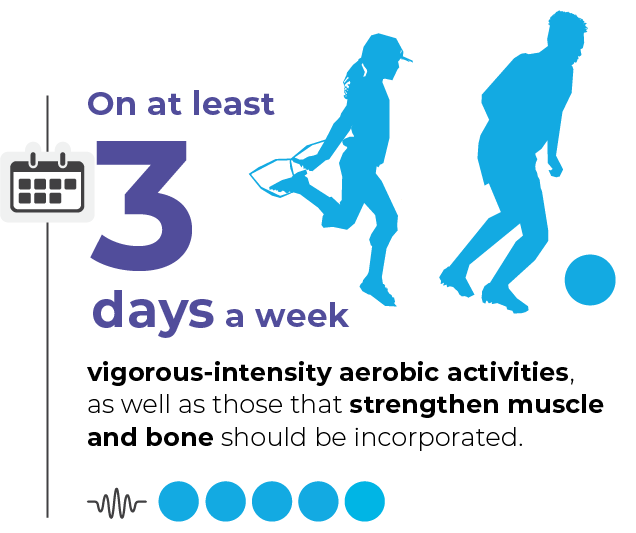
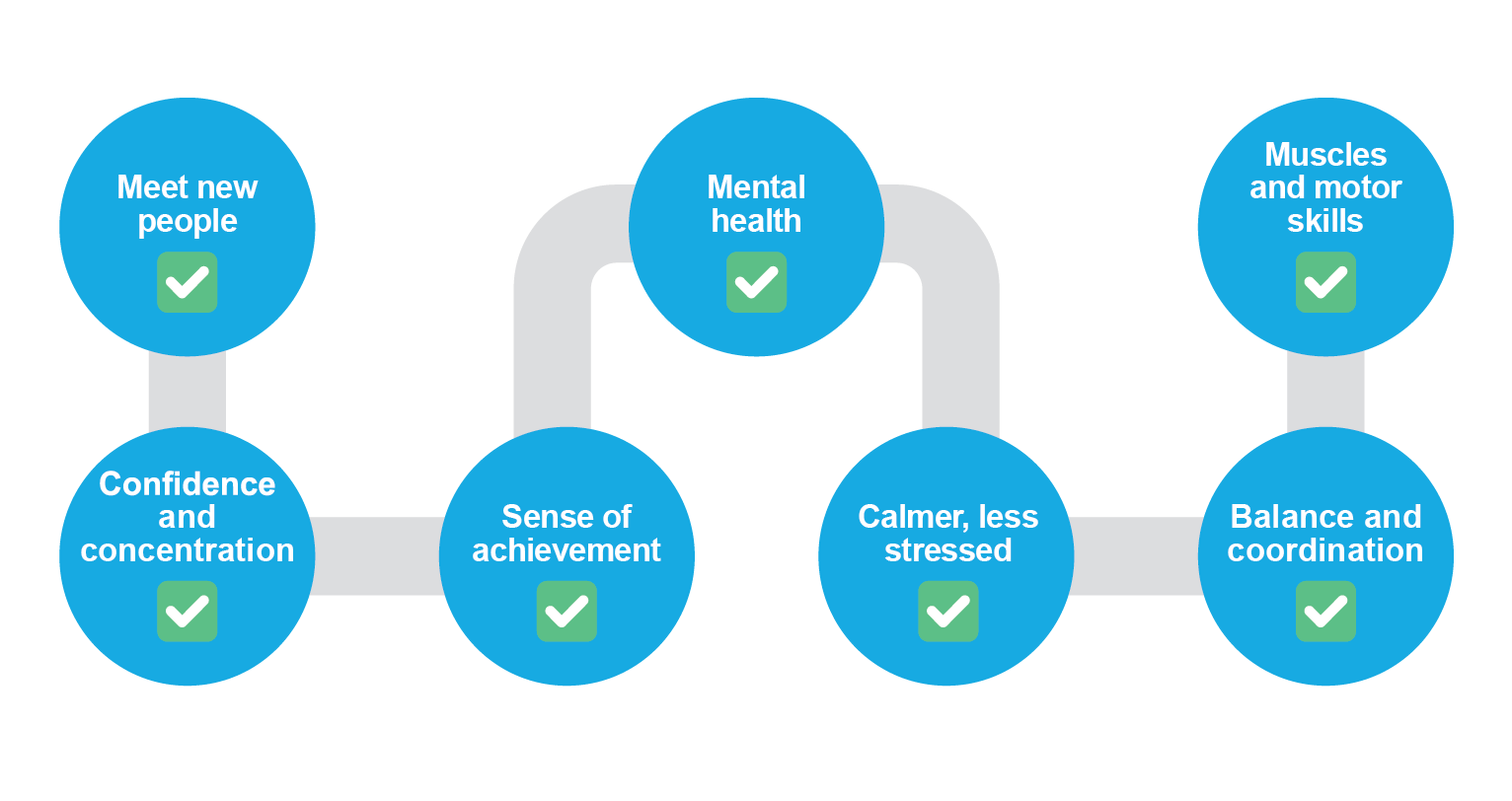
In children and adolescents, physical activity confers benefits for the following health outcomes: improved physical fitness (cardiorespiratory and muscular fitness), cardiometabolic health (blood pressure, dyslipidaemia, glucose, and insulin resistance), bone health, cognitive outcomes (academic performance, executive function), mental health (reduced symptoms of depression); and reduced adiposity.
Good Practice Statements
- Doing some physical activity is better than doing none.
- If children and adolescents are not meeting the recommendations, doing some physical activity will benefit their health.
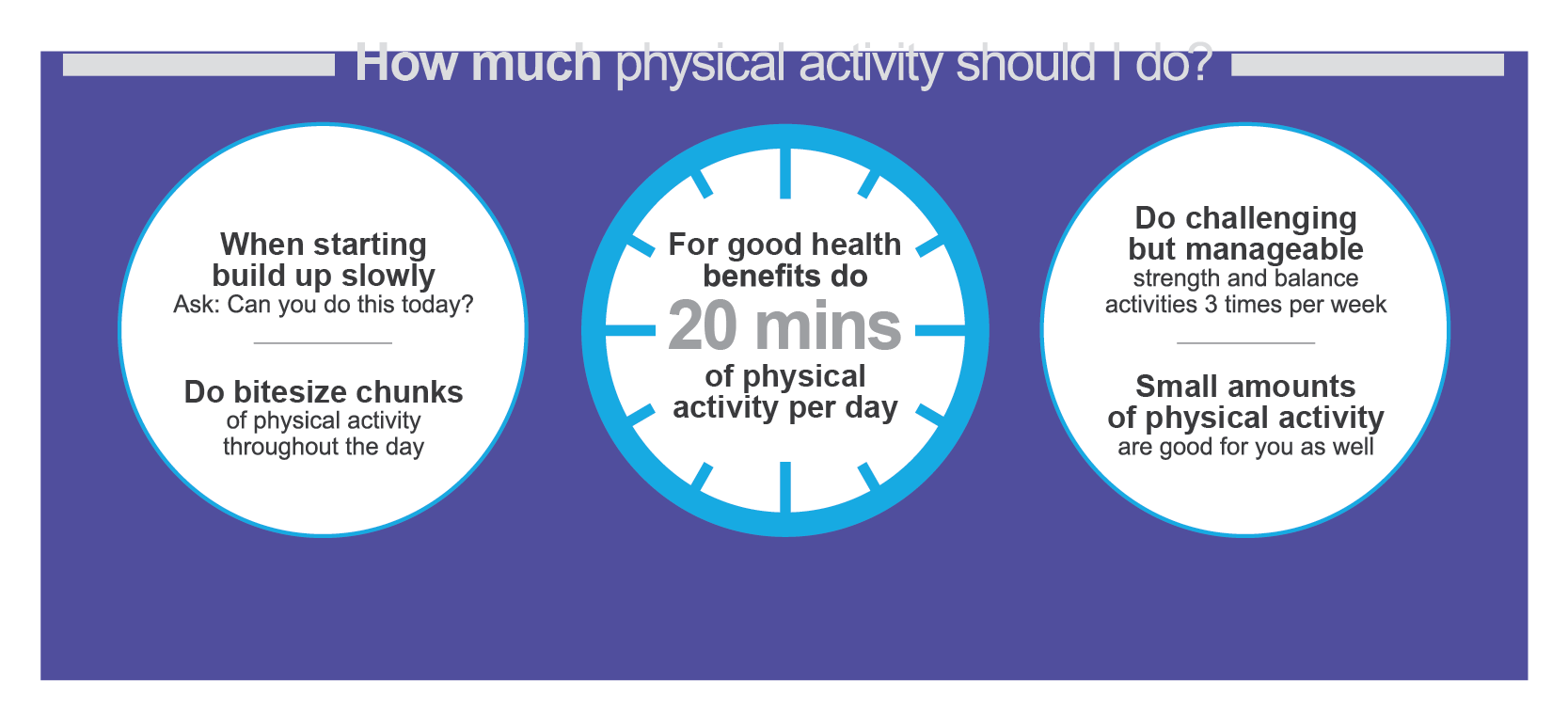
- Children and adolescents should start by doing small amounts of physical activity, and gradually increase the frequency, intensity and duration over time.
- It is important to provide all children and adolescents with safe and equitable opportunities, and encouragement, to participate in physical activities that are enjoyable, offer variety, and are appropriate for their age and ability.
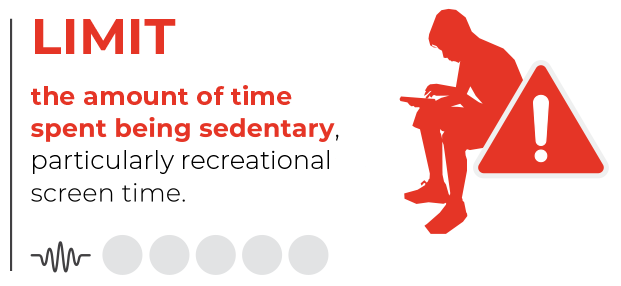
In children and adolescents, higher amounts of sedentary behaviour are associated with the following poor health outcomes: increased adiposity; poorer cardiometabolic health, fitness, behavioural conduct/pro-social behaviour; and reduced sleep duration.
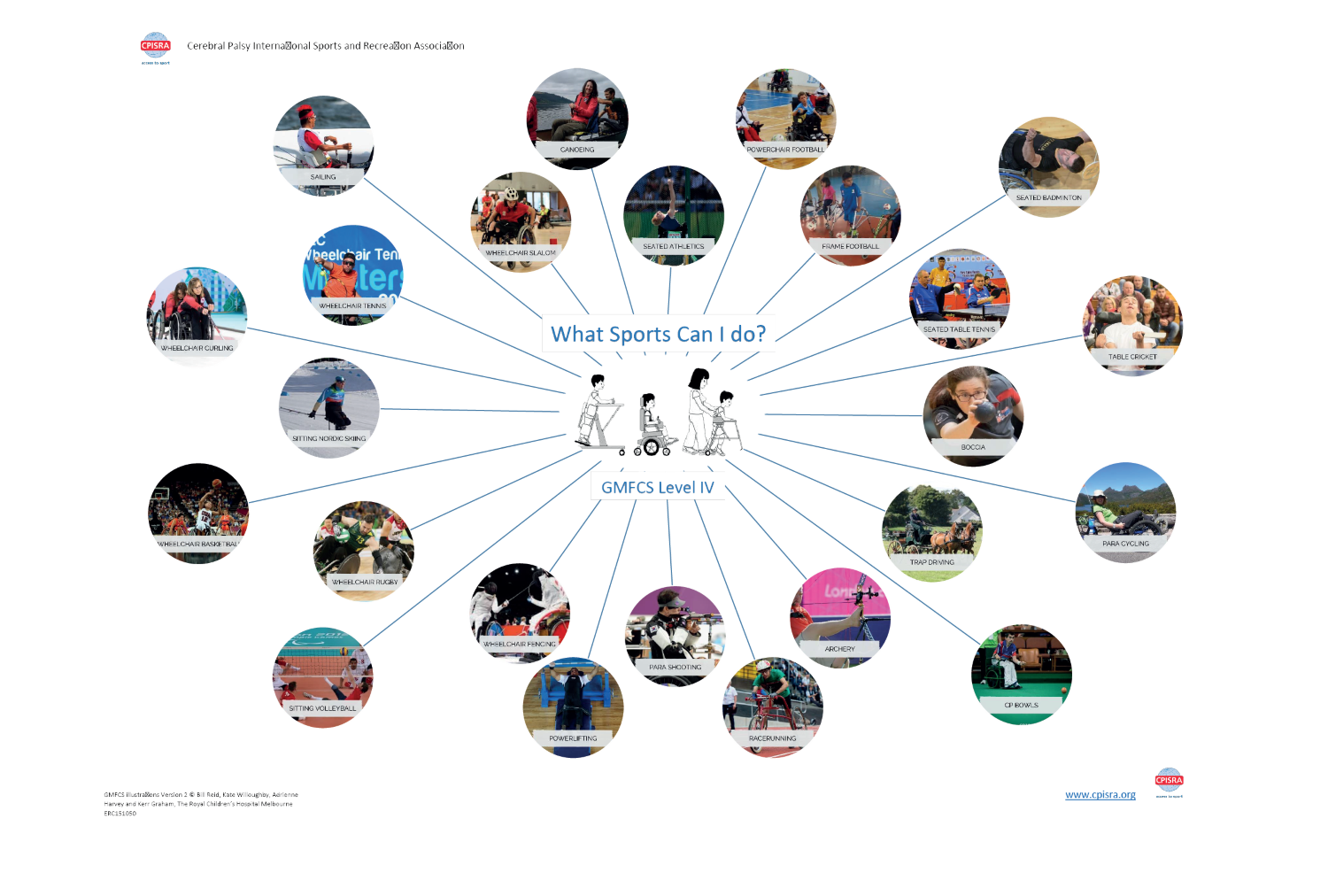
Physical Activity for Disabled Children and Disabled Young People
UK Chief Medical Officers’ Physical Activity Guidelines for Disabled Children and Disabled Young People 2022. This infographic was co-produced with disabled children, disabled young people, parents and carers.
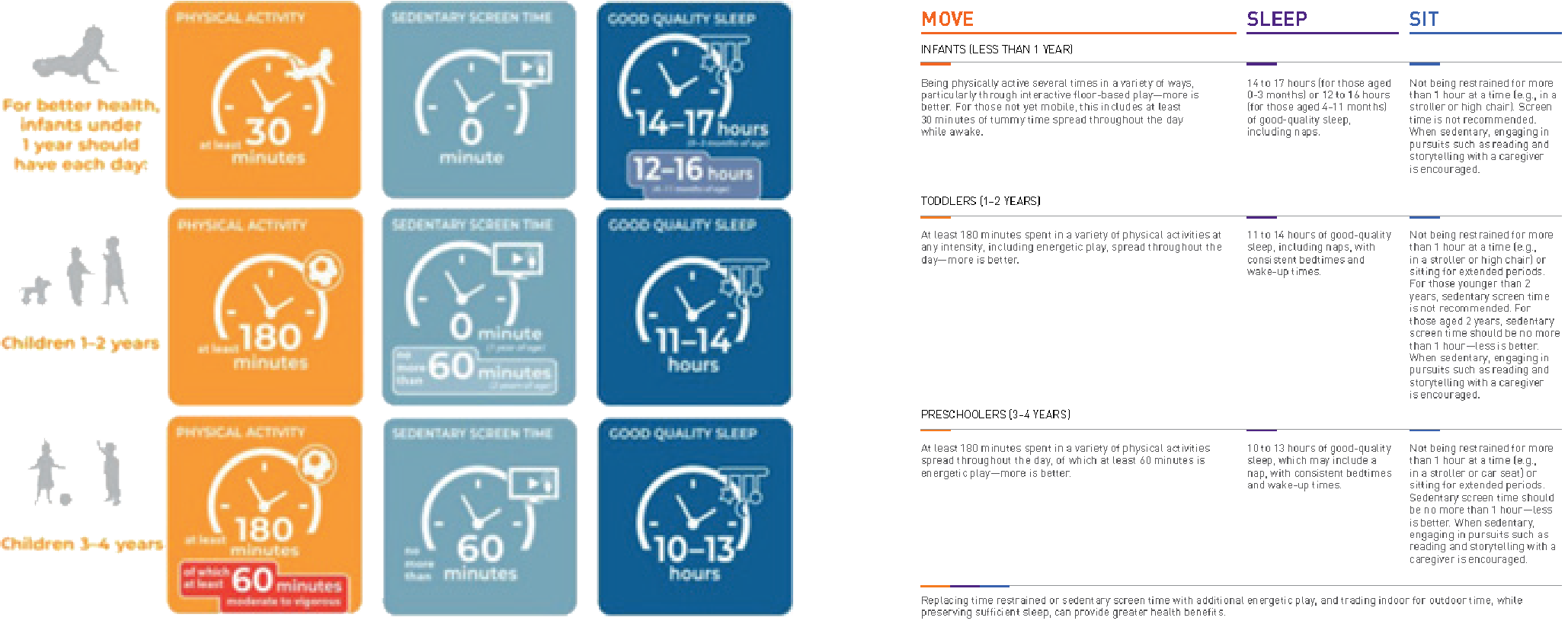
EARLY YEARS – The movement needs of children under the age of 5 are different to those of older children and
SLEEP adolescents, owing to the nature of a child’s growth and early development. Infants and toddlers require more sleep,
and physical activity should be based around play, development of skills, experience, and learning. Early childhood is typically a period of rapid physical and cognitive development and children and infants have remarkable brain plasticity and a natural ability to learn. A child’s habits are formed quickly and family lifestyle habits are open to changes and adaptations in infanthood. Forming good movement behaviours early on can help set up a good structure for later in life, as it is harder to change behaviour and routines that have already become established. Thinking specifically about postural care and physical developmental milestones, it should be encouraged that a child with physical disability is supported in experiencing the same movement as their typically developing peers, so long as it is appropriate, and any risks are managed. Expert clinical recommendations often encourage postural care programmes that encourage postural activity from an early age. Postural care in lying is recommended as soon as is appropriate after birth for the most severe movement impairments in those with Cerebral Palsy:
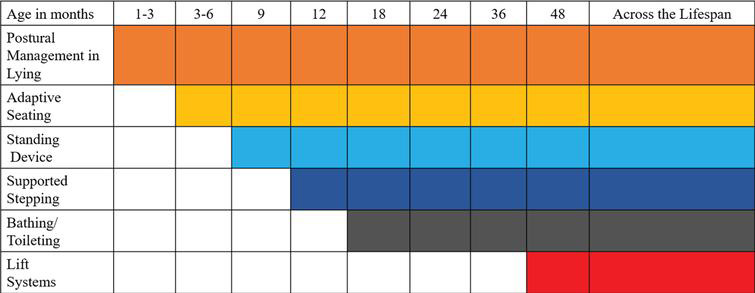
Image from: Paleg, G. & Livingstone, R. Evidence-informed clinical perspectives on postural management for hip health in children and adults with
non-ambulant cerebral palsy. Journal of Pediatric Rehabilitation Medicine: An Interdisciplinary Approach Throughout the Lifespan. 2022; 15(1): 39–48.
Support from a multidisciplinary team is therefore essential in ensuring an individualised programme is established for the child and so that families and carers can understand and engage in the benefits of early intervention, postural care and therapeutic equipment. World Health Organisation and Canadian 24-hour movement advice for children under 5:
 Ei Smart provide brilliant resources for age – appropriate play to support child development – and the leaflets are available in multiple languages!
Ei Smart provide brilliant resources for age – appropriate play to support child development – and the leaflets are available in multiple languages!
https://eismart.co.uk/resources/#podcasts-leaflets
Think about your typical daily routine/ the typical daily routine of the child you care for. How much physical activity, sedentary behaviour and sleep are you/they getting throughout this typical day?
Knowing what is vigorous or light physical activity can be challenging in children with disability, particularly those with more complex needs. It can also be difficult to remember exactly what activity you/they have done throughout the day. Therefore, it is encouraged that this 24-hour clock is completed in collaboration between the child, their carers, their health professionals, and their teaching staff.
Colour this 24 hour clock using the shading key provided to highlight the different levels of activity you/your child partakes in through the day. Remember as a general guide – moderate to vigorous physical activities require physical effort and should make you/your child or teen feel more tired and breathe harder than usual, light physical activity requires smaller effort and movement of any body parts can equal light physical activity, sedentary behaviour is a static activity with minimal body movement and energy use.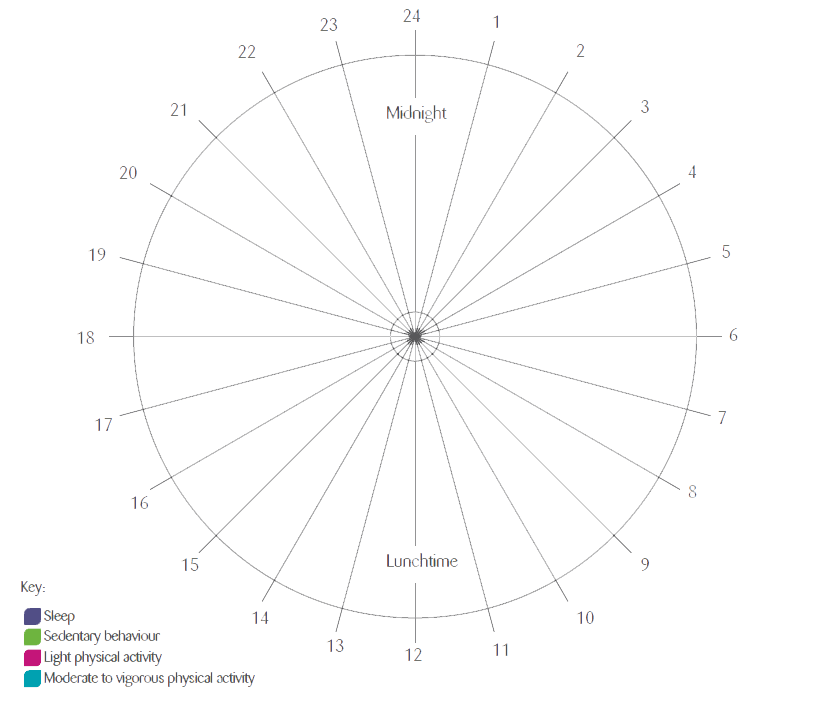
The F-Words build upon the World Health Organisation’s ICF Framework and includes key areas of a child’s development. Recognising that no one factor is more important than another, this can help guide clinical decision making and encourage more holistic, child and carer–centred approaches.